New York
COVID-19 is not the only respiratory infection the globe has been fighting, especially in the colder months. Last winter, the flu nearly disappeared worldwide because precautions taken against COVID-19, including masks and social distancing, also worked to prevent it.
These precautions may have been especially powerful against the flu because they were layered upon some protective immunity people had built up from years of prior exposure to various flu viruses. There was no such protection from COVID-19, which was novel.
This year could be different, as people return to their usual activities and precautions are relaxed. But by embracing what’s been learned from SARS-CoV-2, the coronavirus that causes COVID-19 — including newer thinking on how respiratory viruses spread in general — the world can change the trajectory of flu seasons, potentially saving tens of thousands of lives in the process.
When COVID-19 first appeared, public health authorities worried mainly about the new coronavirus spreading through large fluid droplets — like from a cough or a sneeze. The guidance for individual behavior followed: Wash your hands, stay six feet apart and maybe even wipe down your groceries.
But a detailed understanding of flu transmission — developed over decades and recognised by precious few scientists until recently — laid the basis for scientists’ awakening to the reality of airborne transmission of SARS-CoV-2.
Research has found that, as with SARS-CoV-2, flu virus is exhaled in small particles by infected people while breathing, talking and coughing; and the flu virus has been found in aerosols in indoor environments, including hospitals, children’s day care centers and airplanes. As with the new coronavirus, people can spread the flu even when they don’t have symptoms, which is further indication that transmission can occur without coughing or sneezing and doesn’t require large, wet droplets.
If recommendations to combat the flu continue to rely heavily on hand washing and surface cleaning, without recognising the role of aerosols in transmission, we are unlikely to make a dent in the 12,000 to 52,000 deaths in the United States per year caused by the flu. But if we take a page from the COVID-19 playbook, the United States could drive flu cases down and prevent missed days of school and work, as well as death.
People who want to prevent flu infection should get their seasonal flu vaccine. They should also now feel more comfortable using masks. The use of masks, along with washing hands, appears to reduce transmission of flu to others within households. Those concerned about flu infections may also want to consider limiting the time spent during flu season in crowded indoor settings, where transmission can happen more easily.
I’ll admit, this is hard to do around the holidays, when we want to gather with others, but it is an effective way to reduce risk. The most important message is that if you feel sick, even if just a little bit, stay home so that you don’t spread disease to others.
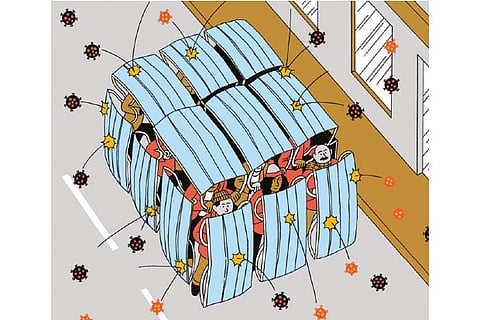
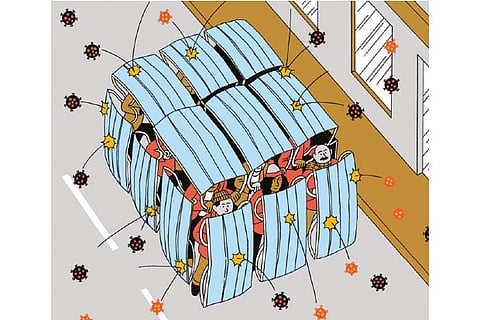
Realistically, people will be spending time indoors with others this season with and without masks. But not every indoor space poses the same level of risk. Spaces with poor ventilation can be more worrisome.
It took a long time for air cleaning to be recognised as a powerful tool for reducing the risk of COVID-19 transmission, and it should be embraced more thoroughly during this pandemic and to reduce flu cases. Ventilation and filtration are two proven techniques for physically removing viruses from the air, so that people are exposed to fewer of them. Poor ventilation was a factor in many coronavirus superspreading events, such as the outbreak at a choir practice in Skagit Valley, Wash.
There are some simple ways to improve ventilation, like opening windows and doors. A recent small study, which has not yet been peer-reviewed, showed that the amount of coronavirus in the air was substantially lowered when ventilation was significantly increased by running an exhaust fan that removed stale air from a room, pulling in outside air through an open window. Other effective options can require more effort. Ultraviolet treatment is another approach used in hospitals to kill viruses in the air. This technique could be more broadly applied in crowded public areas, although it must be properly installed to be effective and avoid the potential for harm. The initial cost is higher than other approaches, but it is worth considering as part of a cost-benefit analysis of different technologies.
Increasing humidity may also be helpful for reducing transmission. The evidence isn’t as strong as for the other tools, but some data show that humidifying the air in the range of 40 to 60 percent — but not higher because that promotes mold growth — could help. In this range, certain flu viruses, the new coronavirus and other viruses don’t survive as well, and our immune response is stronger than when the air is drier. This effect is still not fully understood and should be researched further. I’ve long believed, based on years of research, that the role of aerosols in the spread of many respiratory viruses is underappreciated by the medical community. I hope that COVID-19 has catalysed a shift in thinking about the air we breathe. You wouldn’t drink a glass of water full of pathogens, chemicals and dirt. Why should we put up with breathing contaminated air?
There are still some unknowns: How much respiratory virus transmission is attributed to inhaling aerosols versus being sprayed with large droplets versus touching contaminated surfaces is unclear. How do we grow that knowledge and design buildings to minimise disease transmission? That’s a question that governments and scientists should address.
It will be a challenge to rethink the design and operation of buildings to account for air quality, but it is not insurmountable. Around the turn of the 20th century, the proliferation and modernisation of water and sewage treatment systems helped make common waterborne diseases such as typhoid and cholera a rarity in the United States and Europe. The results of investments in water infrastructure are considered one of the greatest public health achievements of the 20th century. Making air quality healthier as a way to cut down on disease should be a public health focus for this century.
Visit news.dtnext.in to explore our interactive epaper!
Download the DT Next app for more exciting features!
Click here for iOS
Click here for Android